Introduction
Vitamin D, often called the “sunshine vitamin,” is a fat-soluble nutrient that functions as both a nutrient consumed in food and a hormone the body produces. While it is most famous for its role in bone health, research continually reveals its profound and far-reaching importance in regulating numerous systems throughout the body, from immunity and muscle function to mood and cardiovascular health. Given that deficiency is globally widespread, understanding how to maintain optimal levels is critical for long-term well-being.
The Vital Importance of Vitamin D
The primary and most well-established function of Vitamin D is to maintain the balance of calcium and phosphate in the blood.
-
Bone Health: Vitamin D is essential because it promotes the efficient absorption of calcium and phosphorus from the food we eat in the gut. Without adequate Vitamin D, the body cannot absorb enough calcium, forcing it to pull calcium from the skeletal structure to maintain blood levels, which leads to weak, soft, and brittle bones.
-
Immune System Modulation: Receptors for the active form of Vitamin D (calcitriol) are found on many immune cells, suggesting a key role in the body’s defense mechanisms. It helps reduce inflammation and can enhance the pathogen-fighting effects of immune cells.
-
Muscle and Nerve Function: Vitamin D supports normal muscle contraction and coordination. It is also involved in the function of the nervous system, helping in nerve transmission.
-
Potential Links to Chronic Disease: Low Vitamin D levels have been epidemiologically linked to an increased risk of chronic conditions, including certain cancers, type 2 diabetes, hypertension, and autoimmune diseases like multiple sclerosis.
The Metabolism: How the Body Uses the Sun
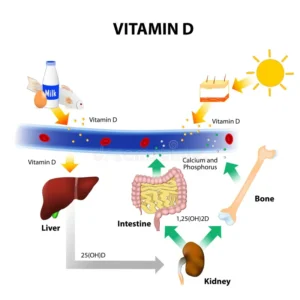
Vitamin D metabolism involves a fascinating two-step process:
-
Synthesis (Skin): When the skin is exposed to UVB sunlight, a cholesterol derivative called 7-dehydrocholesterol is converted into Vitamin D3 (cholecalciferol).
-
Activation (Liver and Kidneys): This inactive Vitamin D3, along with any Vitamin D consumed from diet or supplements, travels to the liver, where it is converted into 25-hydroxyvitamin D (25(OH)D) or calcifediol. This is the main circulating form measured in blood tests. The 25(OH)D is then sent to the kidneys, where it is converted into the active hormone, 1,25-dihydroxyvitamin D (1,25(OH)₂D) or calcitriol, which targets receptors in the gut, bone, and elsewhere to exert its effects.
Deficiency Symptoms: What Happens When Levels Drop
Vitamin D deficiency can be silent for years, but when severe or prolonged, it leads to distinct health consequences:
| Population | Condition/Symptoms | Description |
| Children | Rickets | A rare but serious condition leading to failure of bone tissue to properly mineralize, resulting in soft bones, bowed legs, skeletal deformities, and stunted growth. |
| Adults | Osteomalacia | The adult form of rickets, characterized by softening of the bones, muscle weakness, and chronic, widespread bone and joint pain, often in the lower back and hips. |
| All Ages | General Symptoms | Fatigue, general muscle weakness, aches and cramps, chronic bone pain, and sometimes mood changes like depression. |
Critical Levels in the Body (25-hydroxyvitamin D Blood Test)
The status of Vitamin D is determined by measuring the circulating level of 25(OH)D in the blood, typically reported in nanograms per milliliter (ng/mL) or nanomoles per liter (nmol/L). While optimal ranges can be debated among experts, the following categorizations are widely used by major health organizations for both adults and children:
| 25(OH)D Level (ng/mL) | Health Status | Clinical Implication |
| < 12 | Deficient | High risk for rickets (children) and osteomalacia (adults). Requires medical treatment. |
| 12–19 | Insufficient | Levels are below optimal and require increasing intake through sun, diet, or supplementation to maintain bone health. |
| ≥ 20 | Sufficient/Adequate | Generally considered adequate for bone and overall health in most healthy individuals. |
| ≥ 30 | Optimal/Preferred | Many healthcare providers and experts consider levels of 30–60 ng/mL to be the optimal range for overall health benefits. |
| > 50 | High | Higher than typically needed, and levels >150 ng/mL are associated with toxicity. |
Food Sources and Supplementation
While the sun is the best natural source, geography, season, and lifestyle often make it necessary to rely on diet and supplements.

| Source Category | Examples | Notes |
| Sunlight | Direct midday sun exposure | 10–30 minutes of sun exposure to the arms, legs, and face several times a week, especially in spring and summer, can generate sufficient amounts. |
| Natural Food Sources | Fatty Fish (Salmon, Mackerel, Tuna), Fish Liver Oils (Cod liver oil), Egg Yolks, Beef Liver | Oily fish are the best dietary source. |
| Fortified Foods | Milk (Cow, Soy, Almond), Breakfast Cereals, Orange Juice, Some Yogurts, Margarine | In many countries, milk and cereals are fortified to help boost population intake. |
| Supplements | Cholecalciferol (D3) or Ergocalciferol (D2) | Recommended daily intake (RDA) for most adults and children is 600 IU (15 mcg). Adults over 70 often need 800 IU (20 mcg). Supplements are often necessary for those with limited sun exposure or diagnosed deficiency. |